New tool to revolutionise chronic wound treatment
- Written by iVillage
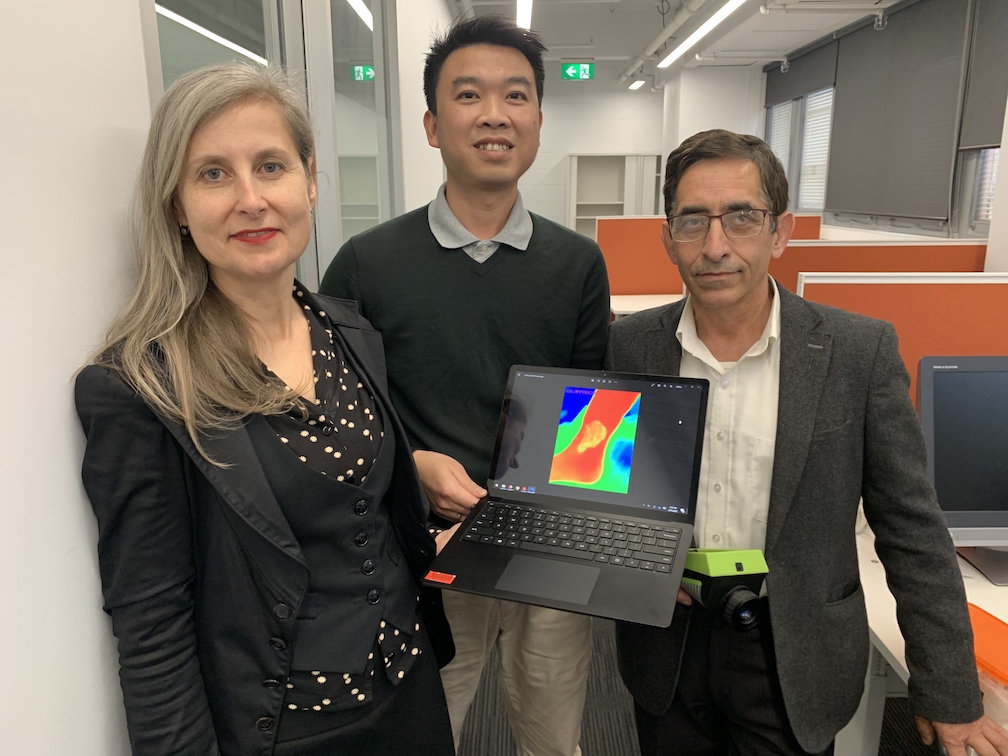
A thermal-imaging tool to screen for chronic wounds could enable nurses to identify these hard-to-heal sores during the first assessment at a person’s home.
Nearly half a million Australians live with chronic wounds, which greatly affect their quality of life and cost the nation’s health system around $3 billion each year.
The latest innovation by researchers at RMIT University and Bolton Clarke Research Institute builds on their team’s work published last year, which enabled the identification of chronic leg sores by the second week after the baseline assessment.
Their latest published results allow the identification of these wounds a week earlier and represents a significant leap forward, the team says.
Lead researcher Professor Dinesh Kumar said their latest clinical study, published in the Nature journal Scientific Reports, presents an AI-powered system to predict how leg ulcers will heal based on thermal images from the first assessment.
“Our new work that identifies chronic leg wounds during the first visit is a world-first achievement,” said Prof Kumar, from RMIT’s School of Engineering. “This means that specialised treatment for slow-healing leg ulcers can begin up to four weeks earlier than the current gold standard.”
Co-researcher, RMIT’s Dr Quoc Cuong Ngo, said while thermal imaging had previously been considered for detecting chronic wounds, the team’s methods enabled significantly earlier detection than other approaches that have been researched.
“Our innovation is not sensitive to changes in ambient temperature and light, so it is effective for nurses to use during their regular visits to people’s homes," he said. “It is also effective in tropical environments, not just here in Melbourne.”
The new method provides information on spatial heat distribution in a wound and predicts, with 78% accuracy, whether leg ulcers would heal in 12 weeks without specialised treatment.
Wounds change significantly over the healing trajectory – higher temperatures signal potential inflammation or infection, while lower temperatures can indicate a slower healing rate due to decreased oxygen in the region.
The research was based on thermal images collected from 56 clients with venous leg ulcers – a type of ulcer associated with poor vein function. This type of ulcer is the most common chronic wound in Australia.
The current gold-standard approach requires taking tracings of the wound size after four weeks, involving physical contact with the wound, which delays identification of slow-healing wounds.
Bolton Clarke Research Institute Senior Research Fellow Dr Rajna Ogrin said the non-contact method reduces infection risk by minimising physical contact.
“Clinical care is provided in many different locations, including specialist clinics, general practices and in people’s homes,” she said. “This method provides a quick, objective, non-invasive way to determine the wound-healing potential of chronic leg wounds that can be used by healthcare providers, irrespective of the setting.
“This means specialised treatments, including advanced wound-cleaning techniques and therapies, can be implemented immediately for problematic leg wounds – up to four weeks earlier than the current gold standard.”
Prof Kumar said, now that the method has been successfully demonstrated in controlled trials with partner clinicians, the next step is to adapt it for a busy nurse or doctor to have this thermal imaging and rapid assessment capability on their mobile phones.
“With the funding we have received from the Medical Research Future Fund, we are now working towards that,” he said. “We are keen to work with prospective partners with different expertise to help us achieve this goal within the next few years.”
The team will also assess whether their method can predict healing of diabetes-related foot ulcers. Untreated chronic wounds in people living with diabetes are the leading cause of limb amputation in Western countries.